Infertility is defined as the inability to conceive after 12 months of unprotected, regular sexual intercourse. It is condition that affects up to one in six couples of reproductive age.
The single biggest influence on a couple’s chances of getting pregnant is woman’s age. Male infertility plays a close second to this, together affecting almost half of all infertile couples.
Causes of infertility are varied and can include:
- Problem with the production of sperm or eggs.
- Structural or functional issues with the female or male reproductive systems.
- Hormone or immune conditions in men, women or both.
Hence it is necessary to get yourself evaluated to find out what is the cause of infertility and treat it accordingly. It is a two pronged approach to look for issues in both the male and female partner.
The first step for couples seeking fertility treatment begins with a thorough assessment of both partners, including a detailed medical history and number of routine tests.
Causes of infertility are varied and can include:
- Problem with the production of sperm or eggs.
- Structural or functional issues with the female or male reproductive systems.
- Hormone or immune conditions in men,women or both.
Sometimes fertility specialists also perform additional tests, including a hysterosalphingogram (HSG), sonohysterogram or a diagnostic laparoscopy, to better assess the condition of the woman’s fallopian tubes, ovaries and uterus.
The most important diagnostic test to assess male infertility is a semen analysis. In nearly all cases, man does not display any obvious outward signs or symptoms that may indicate an issue with his fertility.
Specialist Andrology assessment of sperm is essential to measure:
- The number of sperm, volume and consistency of the sample.
- The size and shape (morphology) and ability to move (mobility) of the sperm, both of which can interfere with penetration and fertilization of an egg.
Male Infertility Evaluation and Treatment
Male-factor infertility alone is responsible for infertility in about 30% of cases, and can contribute to infertility in another 20% of cases. This means that there is some degree of male-factor infertility in up to half of infertility cases.
Male infertility evaluation involves testing whether enough sperm of good quality are being produced and whether it’s getting to where it needs to go to fertilise an egg and produce a pregnancy.
A thorough medical history is a very important part of the male’s workup of infertility. Gathering information about current and past events and conditions can help show what might be contributing to infertility. The various aspects which may be relevant include Fever, Childhood diseases, Undescended testicle, The timing of puberty, Infections, Surgery, Trauma, Sexual history, Exposure to Chemicals /toxins, Drug/Tobacco/Alcohol use, Hot tub/Sauna use, and Respiratory illness.
Once the history is complete, a complete physical exam will be done. This includes checking for the development of secondary sexual characteristics, any signs of hormonal imbalance and examination of male genitalia.
The next step is the semen analysis. This will tell us if there are enough sperm that move and are shaped normally. The morphology of the sperms will point towards its ability to fertilize the ovum. In some men, semen can flow into the bladder. This can be seen by collecting a urine sample immediately after ejaculation for men with low semen volumes and low numbers or absence of sperm.
In case of abnormal semen analysis, it may be helpful to check hormone levels, such as follicle stimulating hormone, testosterone and luteinizing hormone. About 3% of infertile men have a hormone disorder. High hormone levels can result in very low production of sperm or even no sperm. Low hormone levels can indicate congenital conditions or the use of anabolic steroids. Approximately 15% of infertile men with no sperm or very low sperm counts have a genetic abnormality that can be found through genetic testing.
Male infertility treatment will address the specific problem you have. Some fertility treatments require surgery such as Varicocelectomy, Microsurgical Reconstruction for Vasectomy and other blockages, Surgical Sperm Retrieval from testis or epididymis or Transurethral Resection of the Ejaculatory Ducts (TURED). The other treatments involve assisted sperm collection and Assisted Ejaculation.
If problems with ejaculation are present, you may be advised to freeze a semen sample prior to the treatment cycle of the female partner. This sample can be thawed and used when required.
Medications are sometimes used to treat male infertility. Antioxidant therapy (i.e., zinc, vitamin E, vitamin C, L-carnitine, N-acetylcysteine, etc.) may improve pregnancy and live birth rate in couples with male infertility.
Depending on the cause for infertility, intrauterine insemination (IUI) or assisted reproductive techniques are used to help achieve pregnancy.
Each of these treatments comes with its own cost and risks. It is necessary you discuss the most suitable course of treatment with your fertility expert.
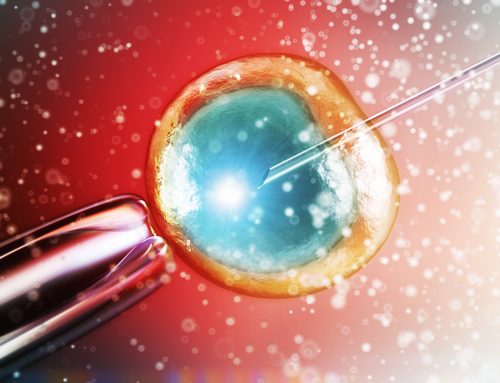
IVF (In vitro fertilization): or test tube baby as it is commonly called is a procedure in which eggs and the sperms are fertilized outside the body and then transferred back to the womb after 2-5 Days.
IVF may be considered if,
- You have been diagnosed with unexplained infertility
- Your fallopian tubes are blocked
- Other techniques such as fertility drugs or intrauterine insemination (IUI) have not been successful
- The male partner has fertility problems and an abnormal semen analysis
- You are using your partner’s frozen sperm in your treatment and IUI is not suitable for you
- You are using donated eggs or your own frozen eggs in your treatment
- You are using embryo testing to avoid passing on a genetic condition to your child.
- You have severe endometriosis
The treatment cycle would be as follows:
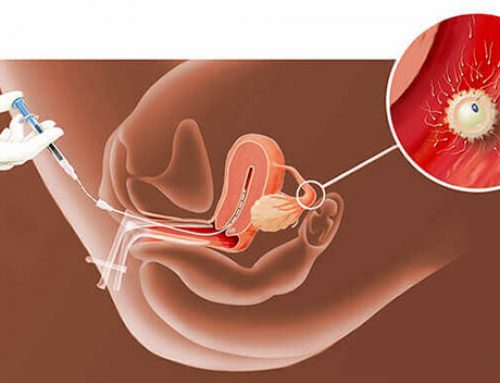
Step 1: Once you have decided to go ahead with IVF, you will undergo a day care procedure called hysteroscopy to assess the suitability of the uterus to hold the baby. It is generally done one month before your IVF cycle and involves the introduction of a small camera into the womb through the vagina to visualize the inside of the uterus. You will be given anesthesia during the procedure and hence there will be no pain.
Step 2: Your husband has to freeze one semen sample as a backup.
Step 3: Typically your treatment would begin on the second or third day of periods. It involves a scan and hormone tests followed by daily injections for about 8-10 days, along with monitoring by scan and hormone tests in between. Once the eggs are sufficiently grown as per the scan and hormone tests, you will receive injection Hcg as a ovulation trigger.
Step 4: Egg retrieval is performed transvaginally 35 – 36 hours later, with light anesthesia, using a transvaginal ultrasound guidance. You will be discharged same evening, unless there are problems associated with bleeding, undue pain or ovarian hyperstimulation.
Step 5: After retrieval, eggs are assessed for their maturity. Meanwhile husband has to give a fresh semen sample. Mature eggs are injected with the sperms on the same day and grown in the incubator for 3-5 days.
Step 6: The final step is the embryo transfer. 3-5 days after your egg retrieval, two or three embryos are selected and gently transferred into the womb using an abdominal ultrasound guidance. The procedure is usually painless, no anesthesia is required and you will be discharged in about two to three hours.
Step 7: You will be given certain supportive medications starting from the day of egg retrieval till your pregnancy check. You will be called for a pregnancy check 16-17 days after your embryo transfer.



Leave A Comment
You must be logged in to post a comment.