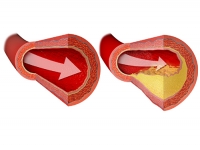
Coronary artery atherosclerosis can be fatal for both men and women. It is the principal cause of coronary artery disease (CAD), in which atherosclerotic changes are present within the walls of the coronary arteries.
Signs and symptoms
The signs and symptoms of coronary artery atherosclerosis include the following:
- Chest pain
- Shortness of breath
- Weakness, tiredness, reduced exertional capacity
- Dizziness, palpitations
- Leg swelling
- Weight gain
- Diaphoresis
- Stable angina pectoris
- Intermittent claudication
- Mesenteric angina
- Tachycardia: Common in persons with acute coronary syndrome (ACS) and acute myocardial infarction (AMI)
- High or low blood pressure
- S 4 gallop: A common early finding
- S 3 gallop: An indication of reduced left ventricular function
- Heart murmurs
- Tachypnea
- Xanthelasmas
- Livedo reticularis
- Syncope
- Leg edema
- Rales
Diagnosis
Laboratory tests:
- Complete blood count (CBC)
- Chemistry panel
- Lipid profile
- Thyroid function tests: To exclude thyroid disorders
- Blood glucose and hemoglobin A 1C (HbA 1C) measurement: Appropriate in patients with diabetes mellitus
- Myocardial fractional flow reserve (FFR)
- Coronary flow reserve (CFR)
- Lipid studies
- C-reactive protein level
- Serum markers
Imaging studies:
- Echocardiography
- Nuclear imaging
- Computed tomography
- Electron beam CT scanning
- Optical coherence tomography imaging
- Magnetic resonance imaging
- Positron emission tomography
- Coronary angiography
- Doppler velocity probes
- Ultrasonography
Management
The following are used in the management of angina
- Nitrates
- Beta blockers
- Statins
- Calcium channel blockers
- Ranolazine
Other agents used in the treatment of coronary artery stenosis or to aid in the management of stable coronary artery disease after intervention include the following:
- Angiotensin-converting enzyme inhibitors to reduce blood pressure
- Antiplatelet agents for acute coronary events
- Intravenous glycoprotein IIb/IIIa inhibitors
- Aspirin
- Clopidogrel
- Ticlopidine
- HMG-CoA reductase inhibitors, or statins to lower LDL cholesterol levels
Treatment procedures for coronary artery atherosclerosis include the following:
- Coronary artery bypass grafting (CABG)
- Percutaneous coronary intervention (PCI)
- Partial ileal bypass
In high- and intermediate-risk patients with 3-vessel disease, PCI was associated with significantly higher rates of revascularization and of major adverse cardiac and cerebrovascular events than CABG; the 2 procedures were equally effective in the treatment of low-risk patients with 3-vessel disease and in low- and intermediate-risk patients with left main CAD.
Treatment
The treatment goals for patients with coronary artery atherosclerosis are to relieve symptoms of coronary artery disease (CAD) and to prevent future cardiac events, such as unstable angina, AMI, and death. The mainstays of pharmacologic therapy of angina include nitrates, beta-blockers, statins, calcium-channel blockers, and ranolazine. Cardiologists in Kolkata suggest that the prevention and treatment of atherosclerosis requires control of the known modifiable risk factors for this disease. This includes therapeutic lifestyle changes and the medical treatment of hypertension, hyperlipidemia, and diabetes mellitus.
Typically, patients with CAD are first seen after they present with a cardiac event. The main focus of their treatment is the index event. The past 4 decades have witnessed tremendous progress in the areas of acute cardiac care, coronary care unit expansion, thrombolytic usage, and PCI. Nevertheless, prevention of cardiac events is likely to have the largest impact on decreasing the burden of atherosclerosis.
High-risk subgroups, in particular, can be targeted for early intervention. Grover and colleagues showed statin therapy in diabetic patients without CAD to be as cost-effective as statin therapy in nondiabetic patients with CAD. Pharmacotherapeutic strategies that affect the risk factor profile, such as the administration of statins for low-density lipoprotein (LDL) reduction or the administration of agents that alter atherosclerotic plaque, are of paramount importance.
Statin Monotherapy vs Combination Therapy
In a systematic review using data from 36 randomized, controlled trials, Gudzune et al concluded that in patients who cannot tolerate or do not respond to high-intensity statin monotherapy, combination therapy using lower-intensity statin therapy in combination with a bile acid sequestrant or with ezetimibe should be considered, albeit cautiously.
According to the heart specialists, in high-risk patients with hyperlipidemia, a combination of low-intensity statin therapy and a bile acid sequestrant produces a 0-14% greater reduction in low-density lipoprotein cholesterol (LDL-C) than does mid-intensity statin monotherapy. [52, 53] Similarly, it was found that compared with high-intensity statin monotherapy, mid-intensity statin therapy combined with ezetimibe results in a 5-15% greater reduction in LDL-C in patients with atherosclerotic cardiovascular disease and a 3-21% greater LDL-C reduction in patients with diabetes.
The investigators urged caution, however, in the use of the above combination therapies, because the trials used in the report lacked data on the long-term benefits and risks of such treatment.




Leave A Comment
You must be logged in to post a comment.